PSYCHIATRIC DRUGS:
Cure or Quackery?
by Lawrence
Stevens, J.D.
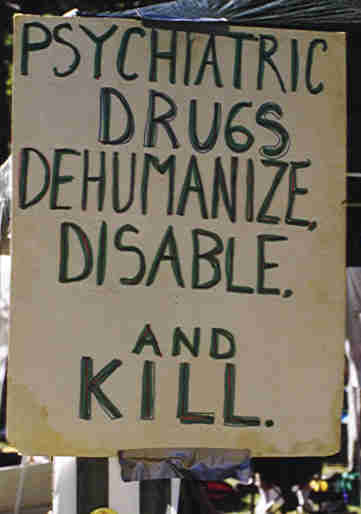
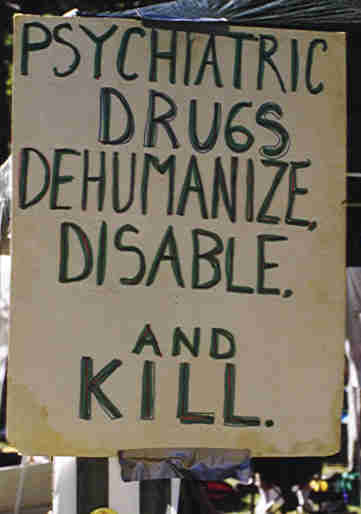
Psychiatric drugs are worthless, and most of them are harmful. Many cause
permanent brain damage at the doses customarily given. Psychiatric drugs and the
profession that promotes them are dangers to your health.
ANTIDEPRESSANTS
The Comprehensive Textbook of Psychiatry/IV, published in 1985, says "The
tricyclic-type drugs are the most effective class of anti-depressants" (Williams
& Wilkins, p. 1520). But in his book Overcoming Depression, published in
1981, Dr. Andrew Stanway, a British physician, says "If anti-depressant drugs
were really as effective as they are made out to be, surely hospital admission
rates for depression would have fallen over the twenty years they've been
available. Alas, this has not happened. ... Many trials have found that
tricyclics are only marginally more effective than placebos, and some have even
found that they are not as effective as dummy tablets" (Hamlyn Publishing Group,
Ltd., p. 159-160). In his textbook Electroconvulsive Therapy, Richard
Abrams, M.D., Professor of Psychiatry at Chicago Medical School, explains the
reason for the 1988 edition of his book updating the edition published 6 years
earlier: "During these six years interest in ECT has bourgeoned. ... What is
responsible for this volte-face in American psychiatry? Disenchantment
with the antidepressants, perhaps. None has been found that is therapeutically
superior to imipramine [a tricyclic], now over 30 years old, and the more
recently introduced compounds are often either less effective or more toxic than
the older drugs, or both" (Oxford Univ. Press, p. xi). In this book, Dr. Abrams
says "despite manufacturers' claims, no significant progress in the
pharmacological treatment of depression has occurred since the introduction of
imipramine in 1958" (p. 7). In the Foreword to this book, Max Fink, M.D., a
psychiatry professor at the State University of New York at Stony Brook, says
the reason for increased use of electroconvulsive "therapy" (ECT) as a treatment
for depression is what he calls "Disappointment with the efficacy of
psychotropic drugs" (p. vii). In his book Psychiatric Drugs: Hazards to the
Brain, published in 1983, psychiatrist Peter Breggin, M.D., asserts: "The
most fundamental point to be made about the most frequently used major
antidepressants is that they have no specifically antidepressant effect. Like
the major tranquilizers to which they are so closely related, they are highly
neurotoxic and brain disabling, and achieve their impact through the disruption
of normal brain function. ... Only the `clinical opinion' of drug advocates
supports any antidepressant effect" of so-called antidepressant drugs (Springer
Pub. Co., pp. 160 & 184). An article in the February 7, 1994 Newsweek
magazine says that "Prozac...and its chemical cousins Zoloft and Paxil are no
more effective than older treatments for depression" (p. 41). Most of the people
I have talked to who have taken so-called antidepressants, including Prozac, say
the drug didn't work for them. This casts doubt on the often made claim that
60% or more of the people who take supposedly antidepressant drugs benefit from
them.
LITHIUM
Lithium is said to be helpful for people whose mood repeatedly changes from
joyful to despondent and back again. Psychiatrists call this manic-depressive
disorder or bipolar mood disorder. Lithium was first described as a psychiatric
drug in 1949 by an Australian psychiatrist, John Cade. According to a
psychiatric textbook: "While conducting animal experiments, Cade had somewhat
incidentally noted that lithium made the animals lethargic, thus prompting him
to administer this drug to several agitated psychiatric patients." The textbook
describes this as "a pivotal moment in the history of psychopharmacology"
(Harold I. Kaplan, M.D. & Benjamin J. Sadock, M.D., Clinical Psychiatry,
Williams & Wilkins, 1988, p. 342). However, if you don't want to be lethargic,
taking lithium would seem to be of dubious benefit. A supporter of
lithium as psychiatric therapy admits lithium causes "a mildly depressed,
generally lethargic feeling". He calls it "the standard lethargy" caused by
lithium (Roger Williams, "A Hasty Decision? Coping in the Aftermath of a
Manic-Depressive Episode", American Health magazine, October 1991, p.
20). Similarly, one of my relatives was diagnosed as manic-depressive and was
given a prescription for lithium carbonate. He told me, years later, "Lithium
insulated me from the highs but not from the lows." It should be no surprise a
lethargy-inducing drug like lithium would have this effect. Amazingly,
psychiatrists sometimes claim lithium wards off feelings of depression even
though, if anything, lethargy-inducing drugs like lithium (like most psychiatric
drugs) promote feelings of despondency and unhappiness - even if they are
called antidepressants.
MINOR TRANQUILIZER/ANTI-ANXIETY DRUGS
Among the most widely used psychiatric drugs are the ones called minor
tranquilizers, including Valium, Librium, Xanax, and Halcion. Doctors who
prescribe them say they have calming, anti-anxiety, panic-suppressing effects or
are useful as sleeping pills. Anyone who believes these claims should go to the
nearest library and read the article "High Anxiety" in the January 1993
Consumer Reports magazine, or read Chapter 11 in Toxic Psychiatry
(St. Martin's Press, 1991), by psychiatrist Peter Breggin, both of which allege
the opposite is closer to the truth. Like all or almost all psychiatric drugs,
the so-called minor tranquilizers don't cure anything but are merely
brain-disabling drugs. In one clinical trial, 70 percent of persons taking
Halcion "developed memory loss, depression and paranoia" ("Halcion manufacturer
Upjohn Co. defends controversial sleeping drug", Miami Herald, December
17, 1991, p. 13A). According to the February 17, 1992 Newsweek, "Four
countries have banned the drug outright" (p. 58). In his book Toxic
Psychiatry, psychiatrist Peter Breggin, speaking of the minor tranquilizers,
says "As with most psychiatric drugs, the use of the medication eventually
causes an increase of the very symptoms that the drug is supposed to ameliorate"
(ibid, p. 246).
PSYCHIATRIC DRUGS versus SLEEP: SLEEP
DISTINGUISHED FROM DRUG-INDUCED UNCONSCIOUSNESS
Contrary to the claim major and minor tranquilizers and so-called
antidepressants are useful as sleeping pills, their real effect is to inhibit or
block real sleep. When I sat in on a psychiatry class with a medical
student friend, the professor told us "Research has shown we do not need to
sleep, but we do need to dream." The dream phase of sleep is the critical
part. Most psychiatric drugs, including those promoted as sleeping medications
or tranquilizers, inhibit this critical dream-phase of sleep, inducing a state
that looks like sleep but actually is a dreamless unconscious state - not
sleep. Sleep, in other words, is an important mental activity that is impaired
or stopped by most psychiatric drugs. A self-help magazine advises: "Do not
take sleeping pills unless under doctor's orders, and then for no more than 10
consecutive nights. Besides losing their effectiveness and becoming addictive,
sleep-inducing medications reduce or prevent the dream-stage of sleep necessary
for mental health" (Going Bonkers? magazine, premiere issue, p. 75). In
The Brain Book, University of Rhode Island professor Peter Russell, Ph.D.,
says "During sleep, particularly during dreaming periods, proteins and other
chemicals in the brain used up during the day are replenished" (Plume, 1979, p.
76). Sleep deprivation experiments on normal people show loss of sleep causes
hallucinations if continued long enough (Maya Pines, The Brain Changers,
Harcourt Brace Jovanovich, 1973, p. 105). So what would seem to be the
consequences of taking drugs that inhibit or block real sleep?
MAJOR
TRANQUILIZER/NERUOLEPTIC/ANTI-PSYCHOTIC/ ANTI-SCHIZOPHRENIC DRUGS
Even as harmful as psychiatry's (so-called) antidepressants and lithium and
(so-called) antianxiety agents (or minor tranquilizers) are, they are nowhere
near as damaging as the so-called major tranquilizers, sometimes also called
"antipsychotic" or "antischizophrenic" or "neuroleptic" drugs. Included in this
category are Thorazine (chlorpromazine), Mellaril, Prolixin
 (fluphenazine), Compazine, Stelazine, and Haldol (haloperidol) - and many
others. In terms of their psychological effects, these so-called major
tranquilizers cause misery - not tranquility. They physically, neurologically
blot out most of a person's ability to think and act, even at commonly given
doses. By disabling people, they can stop almost any thinking or behavior the
"therapist" wants to stop. But this is simply disabling people, not therapy.
The drug temporarily disables or permanently destroys good aspects of a person's
personality as much as bad. Whether and to what extent the disability imposed
by the drug can be removed by discontinuing the drug depends on how long the
drug is given and at how great a dose. The so-called major tranquilizer/
antipsychotic/neuroleptic drugs damage the brain more clearly, severely, and
permanently than any others used in psychiatry. Joyce G. Small, M.D., and Iver
F. Small, M.D., both Professors of Psychiatry at Indiana University, criticize
psychiatrists who use "psychoactive medications that are known to have
neurotoxic effects", and speak of "the increasing recognition of long-lasting
and sometimes irreversible impairments in brain function induced by neuroleptic
drugs. In this instance the evidence of brain damage is not subtle, but is
grossly obvious even to the casual observer!" (Behavioral and Brain Sciences,
March 1984, Vol. 7, p. 34). According to Conrad M. Swartz, Ph.D., M.D.,
Professor of Psychiatry at Chicago Medical School, "While neuroleptics relieve
psychotic anxiety, their tranquilization blunts fine details of personality,
including initiative, emotional reactivity, enthusiasm, sexiness, alertness, and
insight. ... This is in addition to side effects, usually involuntary movements
which can be permanent and are hence evidence of brain damage" (Behavioral
and Brain Sciences, March 1984, Vol. 7, pp. 37-38). A report in 1985 in the
Mental and Physical Disability Law Reporter indicates courts in the United
States have finally begun to consider involuntary administration of the
so-called major tranquilizer/antipsychotic/neuroleptic drugs to involve First
Amendment rights "Because...antipsychotic drugs have the capacity to severely
and even permanently affect an individual's ability to think and
communicate" ("Involuntary medication claims go forward", January-February 1985,
p. 26 - emphasis added). In Molecules of the Mind: The Brave New Science of
Molecular Psychology, Professor Jon Franklin observed: "This era coincided
with an increasing awareness that the neuroleptics not only did not cure
schizophrenia - they actually caused damage to the brain. Suddenly, the
psychiatrists who used them, already like their patients on the fringes of
society, were suspected of Nazism and worse" (Dell Pub. Co., 1987, p. 103). In
his book Psychiatric Drugs: Hazards to the Brain, psychiatrist Peter
Breggin, M.D., alleges that by using drugs that cause brain damage, "Psychiatry
has unleashed an epidemic of neurological disease on the world" one which
"reaches 1 million to 2 million persons a year" (op. cit., pp. 109 & 108). In
severe cases, brain damage from neuroleptic drugs is evidenced by abnormal body
movements called tardive dyskinesia. However, tardive dyskinesia is only the
tip of the iceberg of neuroleptic caused brain damage. Higher mental functions
are more vulnerable and are impaired before the elementary functions of the
brain such as motor control. Psychiatry professor Richard Abrams, M.D., has
acknowledged that "Tardive dyskinesia has now been reported to occur after only
brief courses of neuroleptic drug therapy" (in: Benjamin B. Wolman (editor),
The Therapist's Handbook: Treatment Methods of Mental Disorders, Van
Nostrand Reinhold Co., 1976, p. 25). In his book The New Psychiatry,
published in 1985, Columbia University psychiatry professor Jerrold S. Maxmen,
M.D., alleges: "The best way to avoid tardive dyskinesia is to avoid
antipsychotic drugs altogether. Except for treating schizophrenia, they should
never be used for more than two or three consecutive months. What's criminal is
that all too many patients receive antipsychotics who shouldn't" (Mentor, pp.
155-156). In fact, Dr. Maxmen doesn't go far enough. His characterization of
administration of the so-called antipsychotic/anti-schizophrenic/major
tranquilizer/neuroleptic drugs as "criminal" is accurate for all people,
including those called schizophrenic, even when the drugs aren't given long
enough for the resulting brain damage to show up as tardive dyskinesia. The
author of the Preface of a book by four physicians published in 1980, Tardive
Dyskinesia: Research & Treatment, made these remarks: "In the late 1960s I
summarized the literature on tardive dyskinesia ... The majority of
psychiatrists either ignored the existence of the problem or made futile efforts
to prove that these motor abnormalities were clinically insignificant or
unrelated to drug therapy. In the meantime the number of patients affected by
tardive dyskinesia increased and the symptoms became worse in those already
afflicted by this condition. ... there are few investigators or clinicians who
still have doubts about the iatrogenic [physician caused] nature of tardive
dyskinesia. ... It is evident that the more one learns about the toxic effects
of neuroleptics on the central nervous system, the more one sees an urgent need
to modify our current practices of drug use. It is unfortunate that many
practitioners continue to prescribe psychotropics in excessive amounts, and that
a considerable number of mental institutions have not yet developed a policy
regarding the management and prevention of tardive dyskinesia. If this book,
which reflects the opinions of the experts in this field, can make a dent in the
complacency of many psychiatrists, it will be no small accomplishment" (in:
William E. Fann, M.D., et al., Tardive Dyskinesia: Research & Treatment,
SP Medical & Scientific). In Psychiatric Drugs: Hazards to the Brain,
psychiatrist Peter Breggin, M.D., says this: "The major tranquilizers are highly
toxic drugs; they are poisonous to various organs of the body. They are
especially potent neurotoxins, and frequently produce permanent damage to the
brain. ... tardive dyskinesia can develop in low-dose, short-term usage... the
dementia [loss of higher mental functions] associated with the tardive
dyskinesia is not usually reversible. ... Seldom have I felt more saddened or
more dismayed than by psychiatry's neglect of the evidence that it is causing
irreversible lobotomy effects, psychosis, and dementia in millions of patients
as a result of treatment with the major tranquilizers"(op. cit., pp. 70, 107,
135, 146).
(fluphenazine), Compazine, Stelazine, and Haldol (haloperidol) - and many
others. In terms of their psychological effects, these so-called major
tranquilizers cause misery - not tranquility. They physically, neurologically
blot out most of a person's ability to think and act, even at commonly given
doses. By disabling people, they can stop almost any thinking or behavior the
"therapist" wants to stop. But this is simply disabling people, not therapy.
The drug temporarily disables or permanently destroys good aspects of a person's
personality as much as bad. Whether and to what extent the disability imposed
by the drug can be removed by discontinuing the drug depends on how long the
drug is given and at how great a dose. The so-called major tranquilizer/
antipsychotic/neuroleptic drugs damage the brain more clearly, severely, and
permanently than any others used in psychiatry. Joyce G. Small, M.D., and Iver
F. Small, M.D., both Professors of Psychiatry at Indiana University, criticize
psychiatrists who use "psychoactive medications that are known to have
neurotoxic effects", and speak of "the increasing recognition of long-lasting
and sometimes irreversible impairments in brain function induced by neuroleptic
drugs. In this instance the evidence of brain damage is not subtle, but is
grossly obvious even to the casual observer!" (Behavioral and Brain Sciences,
March 1984, Vol. 7, p. 34). According to Conrad M. Swartz, Ph.D., M.D.,
Professor of Psychiatry at Chicago Medical School, "While neuroleptics relieve
psychotic anxiety, their tranquilization blunts fine details of personality,
including initiative, emotional reactivity, enthusiasm, sexiness, alertness, and
insight. ... This is in addition to side effects, usually involuntary movements
which can be permanent and are hence evidence of brain damage" (Behavioral
and Brain Sciences, March 1984, Vol. 7, pp. 37-38). A report in 1985 in the
Mental and Physical Disability Law Reporter indicates courts in the United
States have finally begun to consider involuntary administration of the
so-called major tranquilizer/antipsychotic/neuroleptic drugs to involve First
Amendment rights "Because...antipsychotic drugs have the capacity to severely
and even permanently affect an individual's ability to think and
communicate" ("Involuntary medication claims go forward", January-February 1985,
p. 26 - emphasis added). In Molecules of the Mind: The Brave New Science of
Molecular Psychology, Professor Jon Franklin observed: "This era coincided
with an increasing awareness that the neuroleptics not only did not cure
schizophrenia - they actually caused damage to the brain. Suddenly, the
psychiatrists who used them, already like their patients on the fringes of
society, were suspected of Nazism and worse" (Dell Pub. Co., 1987, p. 103). In
his book Psychiatric Drugs: Hazards to the Brain, psychiatrist Peter
Breggin, M.D., alleges that by using drugs that cause brain damage, "Psychiatry
has unleashed an epidemic of neurological disease on the world" one which
"reaches 1 million to 2 million persons a year" (op. cit., pp. 109 & 108). In
severe cases, brain damage from neuroleptic drugs is evidenced by abnormal body
movements called tardive dyskinesia. However, tardive dyskinesia is only the
tip of the iceberg of neuroleptic caused brain damage. Higher mental functions
are more vulnerable and are impaired before the elementary functions of the
brain such as motor control. Psychiatry professor Richard Abrams, M.D., has
acknowledged that "Tardive dyskinesia has now been reported to occur after only
brief courses of neuroleptic drug therapy" (in: Benjamin B. Wolman (editor),
The Therapist's Handbook: Treatment Methods of Mental Disorders, Van
Nostrand Reinhold Co., 1976, p. 25). In his book The New Psychiatry,
published in 1985, Columbia University psychiatry professor Jerrold S. Maxmen,
M.D., alleges: "The best way to avoid tardive dyskinesia is to avoid
antipsychotic drugs altogether. Except for treating schizophrenia, they should
never be used for more than two or three consecutive months. What's criminal is
that all too many patients receive antipsychotics who shouldn't" (Mentor, pp.
155-156). In fact, Dr. Maxmen doesn't go far enough. His characterization of
administration of the so-called antipsychotic/anti-schizophrenic/major
tranquilizer/neuroleptic drugs as "criminal" is accurate for all people,
including those called schizophrenic, even when the drugs aren't given long
enough for the resulting brain damage to show up as tardive dyskinesia. The
author of the Preface of a book by four physicians published in 1980, Tardive
Dyskinesia: Research & Treatment, made these remarks: "In the late 1960s I
summarized the literature on tardive dyskinesia ... The majority of
psychiatrists either ignored the existence of the problem or made futile efforts
to prove that these motor abnormalities were clinically insignificant or
unrelated to drug therapy. In the meantime the number of patients affected by
tardive dyskinesia increased and the symptoms became worse in those already
afflicted by this condition. ... there are few investigators or clinicians who
still have doubts about the iatrogenic [physician caused] nature of tardive
dyskinesia. ... It is evident that the more one learns about the toxic effects
of neuroleptics on the central nervous system, the more one sees an urgent need
to modify our current practices of drug use. It is unfortunate that many
practitioners continue to prescribe psychotropics in excessive amounts, and that
a considerable number of mental institutions have not yet developed a policy
regarding the management and prevention of tardive dyskinesia. If this book,
which reflects the opinions of the experts in this field, can make a dent in the
complacency of many psychiatrists, it will be no small accomplishment" (in:
William E. Fann, M.D., et al., Tardive Dyskinesia: Research & Treatment,
SP Medical & Scientific). In Psychiatric Drugs: Hazards to the Brain,
psychiatrist Peter Breggin, M.D., says this: "The major tranquilizers are highly
toxic drugs; they are poisonous to various organs of the body. They are
especially potent neurotoxins, and frequently produce permanent damage to the
brain. ... tardive dyskinesia can develop in low-dose, short-term usage... the
dementia [loss of higher mental functions] associated with the tardive
dyskinesia is not usually reversible. ... Seldom have I felt more saddened or
more dismayed than by psychiatry's neglect of the evidence that it is causing
irreversible lobotomy effects, psychosis, and dementia in millions of patients
as a result of treatment with the major tranquilizers"(op. cit., pp. 70, 107,
135, 146).
Psychiatry professor Richard Abrams, M.D., has pointed out that
"Tricyclic Antidepressants...are minor chemical modifications of chlorpromazine
[Thorazine] and were introduced as potential neuroleptics" (in: B. Wolman,
The Therapist's Handbook, op. cit., p. 31). In his book Psychiatric
Drugs: Hazards to the Brain, Dr. Breggin calls the so-called antidepressants
"Major Tranquilizers in Disguise" (p. 166). Psychiatrist Mark S. Gold, M.D.,
has said antidepressants can cause tardive dyskinesia (The Good News About
Depression, Bantam, 1986, p. 259).
Why do the so-called patients accept such "medication"? Sometimes they
do so out of ignorance about the neurological damage to which they are
subjecting themselves by following their psychiatrist's advice to take the
"medication". But much if not most of the time, neuroleptic drugs are literally
forced into the bodies of the "patients" against their wills. In his book
Psychiatric Drugs: Hazards to the Brain, psychiatrist Peter Breggin,
M.D., says "Time and again in my clinical experience I have witnessed patients
driven to extreme anguish and outrage by having major tranquilizers forced on
them. ... The problem is so great in routine hospital practice that a large
percentage of patients have to be threatened with forced intramuscular injection
before they will take the drugs" (p. 45).
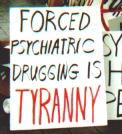
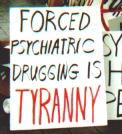
FORCED PSYCHIATRIC TREATMENT COMPARED WITH
RAPE
Forced administration of a psychiatric drug (or a so-called treatment like
electroshock) is a kind of tyranny that can be compared, physically and morally,
with rape. Compare sexual rape and involuntarily administration of a
psychiatric drug injected intramuscularly into the buttocks, which is the part
of the anatomy where the injection usually is given: In both sexual rape
and involuntary administration of a psychiatric drug, force is used. In both
cases, the victim's pants are pulled down. In both cases, a tube is inserted
into the victim's body against her (or his) will. In the case of sexual rape,
the tube is a penis. In the case of what could be called psychiatric rape, the
tube is a hypodermic needle. In both cases, a fluid is injected into the
victim's body against her or his will. In both cases it is in (or near) the
derriere. In the case of sexual rape the fluid is semen. In the case of
psychiatric rape, the fluid is Thorazine, Prolixin or some other brain-disabling
drug. The fact of bodily invasion is similar in both cases if not (for reasons
I'll explain) actually worse in the case of psychiatric rape. So is the sense
of outrage in the mind of the victim of each type of assault. As psychiatry
professor Thomas Szasz once said, "violence is violence, regardless of whether
it is called psychiatric illness or psychiatric treatment." Some who are not
"hospitalized" (that is, imprisoned) are forced to report to a doctor's office
for injections of a long-acting neuroleptic like Prolixin every two weeks by the
threat of imprisonment ("hospitalization") and forced injection of the drug if
they don't comply.
Why is psychiatric rape worse than
sexual rape? As brain surgeon I. S. Cooper, M.D., said in his autobiography:
"It is your brain that sees, feels, thinks, commands, responds. You are your
brain. It is you. Transplanted into another carrier, another body, your
brain would supply it with your memories, your thoughts, your emotions. It
would still be you. The new body would be your container. It would carry you
around. Your brain is you" (The Vital Probe: My Life as a Brain
Surgeon, W.W.Norton & Co., 1982, p. 50-emphasis in original). The most
essential and most intimate part of you is not what is between your legs but
what is between your ears. An assault on a person's brain such as
involuntary administration of a brain-disabling or brain-damaging "treatment"
(such as a psychoactive drug or electroshock or psychosurgery) is a more
intimate and morally speaking more horrible crime than sexual rape. Psychiatric
rape is in moral terms a worse crime than sexual rape for another reason, also:
The involuntary administration of psychiatry's biological "therapies" cause
permanent impairment of brain function. In contrast, women usually are
still fully sexually functional after being sexually raped. They suffer
psychological harm, but so do the victims of psychiatric assault. I hope I will
not be understood as belittling the trauma or wrongness of sexual rape if I
point out that I have counselled sexually raped women in my law practice and
that each of the half-dozen or so women I have known who have been sexually
raped have gone on to have apparently normal sexual relationships, and in most
cases marriages and families. In contrast, the brains of people subjected to
psychiatric assault often are not as fully functional because of the
physical, biological harm done by the "treatment". On a TV talk show in
1990, psychoanalyst Jeffrey Masson, Ph.D., said he hopes those responsible for
such "therapies" will one day face "Nurnburg trials" (Geraldo, Nov. 30,
1990).
BRAIN-DAMAGING PSYCHIATRIC DRUGS ARE
INFLICTED ON NURSING HOME RESIDENTS
These very same brain-damaging (so-called) neuroleptic/antipsychotic drugs are
routinely administered - involuntarily - to mentally healthy old people in
nursing homes in the United States. According to an article in the
September/October 1991 issue of In-Health magazine, "In nursing homes,
antipsychotics are used on anywhere from 21 to 44 percent of the
institutionalized elderly... half of the antipsychotics prescribed for nursing
home residents could not be explained by the diagnosis in the patient's chart.
Researchers suspect the drugs are commonly used by such
 institutions as chemical straightjackets - a means of pacifying unruly patients"
(p. 28). I know of two examples of feeble old men in nursing homes who were
barely able to get out of their wheelchairs who were given a
neuroleptic/antipsychotic drug. One complained because he was strapped into a
wheelchair to prevent his attempts to try to walk with his cane. The other was
strapped into his bed at night to prevent him from getting up and falling when
going to the bathroom, necessitating defecating in his bed. Both were so
physically disabled they posed no danger to anyone. But both dared complain
bitterly about how they were mistreated. In both cases the nursing home staffs
responded to these complaints with injections of Haldol - mentally disabling
these men, thereby making it impossible for them to complain. The use of these
damaging drugs on nursing home residents who are not considered to have
psychiatric problems shows that their real purpose is control, not therapy.
Therapeutic claims for neuroleptic drugs are rationalizations without factual
support.
institutions as chemical straightjackets - a means of pacifying unruly patients"
(p. 28). I know of two examples of feeble old men in nursing homes who were
barely able to get out of their wheelchairs who were given a
neuroleptic/antipsychotic drug. One complained because he was strapped into a
wheelchair to prevent his attempts to try to walk with his cane. The other was
strapped into his bed at night to prevent him from getting up and falling when
going to the bathroom, necessitating defecating in his bed. Both were so
physically disabled they posed no danger to anyone. But both dared complain
bitterly about how they were mistreated. In both cases the nursing home staffs
responded to these complaints with injections of Haldol - mentally disabling
these men, thereby making it impossible for them to complain. The use of these
damaging drugs on nursing home residents who are not considered to have
psychiatric problems shows that their real purpose is control, not therapy.
Therapeutic claims for neuroleptic drugs are rationalizations without factual
support.
SUPPOSEDLY "DOUBLE-BLIND" PSYCHIATRIC DRUG
STUDIES ARE BIASED
Studies indicating psychiatric drugs are helpful are of dubious credibility
because of professional bias. All or almost all psychiatric drugs are
neurotoxic and for this reason cause symptoms and problems such as dry mouth,
blurred vision, lightheadedness, dizziness, lethargy, difficulty thinking,
menstrual irregularities, urinary retention, heart palpitations, and other
consequences of neurological dysfunction. Psychiatrists deceptively call these
"side-effects", even though they are the only real effects of today's
psychiatric drugs. Placebos (or sugar pills) don't cause these problems. Since
these symptoms (or their absence) are obvious to psychiatrists evaluating
psychiatric drugs in supposedly double-blind drug trials, the drug trials aren't
really double-blind, making it impossible to evaluate psychiatric drugs
impartially. This allows professional bias to skew the results.
MODES OF ACTION: UNKNOWN
Despite various unverified theories and claims, psychiatrists don't know how the
drugs they use work biologically. In the words of Columbia University
psychiatry professor Jerrold S. Maxmen, M.D.: "How psychotropic drugs work is
not clear" (The New Psychiatry, Mentor, 1985, p. 143). Experience has
shown that the effect of all of today's commonly used psychiatric drugs is to
disable the brain in a generalized way. None of today's psychiatric
drugs have the specificity (e.g., for depression or anxiety or psychosis) that
is often claimed for them.
LIKE TAKING INSULIN FOR DIABETES?
It is often asserted that taking a psychiatric drug is like taking insulin for
diabetes. Although psychiatric drugs are taken continuously, as is insulin -
it's an absurd analogy. Diabetes is a disease with a known physical cause. No
physical cause has been found for any of today's so-called mental illnesses. The
mode of action of insulin is known: It is a hormone that instructs or causes
cells to uptake dietary glucose (sugar). In contrast, the modes of action of
psychiatry's drugs are unknown - although advocates of psychiatric drugs as well
as critics theorize they prevent normal brain functioning by blocking
neuroreceptors in the brain. If this theory is correct it is another contrast
between taking insulin and taking a psychiatric drug: Insulin restores a
normal biological function, namely, normal glucose (or sugar) metabolism.
Psychiatric drugs interfere with a normal biological function, namely,
normal neuroreceptor functioning. Insulin is a hormone that is found naturally
in the body. Psychiatry's drugs are not normally found in the body. Insulin
gives a diabetic's body a capability it would not have in the absence of
insulin, namely, the ability to metabolize dietary sugar normally. Psychiatric
drugs have an opposite kind of effect: They take away (mental) capabilities the
person would have in the absence of the drug. Insulin affects the body rather
than mind. Psychiatric drugs disable the brain and hence the mind, the mind
being the essence of the real self.
THE AUTHOR, Lawrence Stevens, is a lawyer whose practice has included
representing psychiatric "patients". His pamphlets are not copyrighted. You are
invited to make copies for distribution to those who you think will benefit.
 DOWNLOAD
AS PAMPHLET - Click on this link to download a file from which you can print
a copy of this article, "Psychiatric Drugs: Cure or Quackery?," in pamphlet
form. You will need 8Ĺ by 14 inch paper, a printer capable of Hewlett-Packard
Laserjet (PCL 5) emulation, and Corel WordPerfect for Microsoft Windows 95/98.
Printer capable of duplexing (i.e., double-sided printing) is recommended. See
printing instructions.
Most Kinko's Copy shops in the USA and Canada have the needed hardware and
software, often including a duplexing printer, to download and print pamphlets
from this website.
DOWNLOAD
AS PAMPHLET - Click on this link to download a file from which you can print
a copy of this article, "Psychiatric Drugs: Cure or Quackery?," in pamphlet
form. You will need 8Ĺ by 14 inch paper, a printer capable of Hewlett-Packard
Laserjet (PCL 5) emulation, and Corel WordPerfect for Microsoft Windows 95/98.
Printer capable of duplexing (i.e., double-sided printing) is recommended. See
printing instructions.
Most Kinko's Copy shops in the USA and Canada have the needed hardware and
software, often including a duplexing printer, to download and print pamphlets
from this website.
1997 UPDATE:
The following is an excerpt from "What
is Schizophrenia?" by William C. Wirshing, M.D.:
... 3. Coincident with this observed
antipsychotic effect [of Thorazine] was a curious neurotoxicity
clinically indistinguishable from idiopathic Parkinsonís disease. They [the
drug's discoverers and developers] were, in fact, so impressed with this
correlation that they suggested to their colleagues that patients be dosed
to this 'neuroleptic threshold.' Thus, toxicity fell into a lockstep with
efficacy in the minds of all clinicians and basic researchers who dealt with
these molecules. The task that then fell to the basic researchers and the
medicinal chemists was, 'How does Thorazine work?' The short answer to this
question is that, even after a half century of toil, medical science is
still not quite sure. ... Unfortunately, even in 1997, there is no
way to screen a drug preclinically (i.e., in animal or other nonhuman
models) for antischizophrenic potency. It appears that the liability to get
schizophrenia is uniquely human. The liability, however, to manifest
parkinsonism, on the other hand, is shared by many mammalian species.
Therefore, if the original clinical observation linking neurotoxicity (the
parkinsonism) and antipsychotic efficacy was correct, then all one had to do
is search for a molecule that induced neurotoxicity in animals. When given
to humans, this would not only induce the neurotoxicity but would result in
antipsychotic efficacy. And this is what was done, over and over
again-nearly 250 molecules have been elaborated in roughly this fashion
during the last half century. Said another way, these drugs were discovered
and developed because they produce neurotoxicity in animals. This,
therefore, is their primary effect. Clinicians exploit the fortuitous
co-occurrence of the side effect of antipsychotic potency. It should be no
surprise then that all available "conventional" antipsychotic cornpounds
produce neurotoxicity - this is what they were designed to do. ... 1) All
conventional antipsychotic medications not only shared antipsychotic
potential, they also shared neurotoxic liabilities - they are called, after
all, 'neuroleptics,' which roughly translates as 'neurotoxic.' ... So
then, how does clozapine work? Again, no one knows the answer.
[emphasis added]
The author, Willian C. Wirshing, M.D., is
an associate professor of psychiatry at UCLA Medical School and director of the
Movement Disorders Laboratory at the Brentwood VA Medical Center as well as a
member of The JOURNAL Advisory Board and its medical editor.
1998 UPDATE:
The following statements are made by Michael J. Murphy, M.D., M.P.H., Clinical
Fellow in Psychiatry, Harvard Medical School; Ronald L. Cowan, M.D.,
Ph.D., Clinical Fellow in Psychiatry, Harvard Medical School; and Lloyd
I. Sederer, M.D., Associate Professor of Clinical Psychiatry, Harvard Medical
School, in their textbook Blueprints in Psychiatry (Blackwell Science,
Inc., Malden, Massachusetts, 1998):
Lithium:
"The mechanism of action of lithium in the treatment of mania is not well
determined." (p. 57)
Valproate:
"The mechanism of action of valproate is likely to be its augmentation of
GABA function in the CNS [central nervous system]." (p. 58 - underline added)
Carbamazepine:
"The mechanism of action of carbamazepine in bipolar illness is unknown." (p.
59)
Antidepressants:
"Antidepressants are thought to exert their effects at particular subsets
of neuronal synapses throughout the brain. ... SSRIs [e.g., Prozac, Paxil,
Zoloft] act by binding to presynaptic serotonin reuptake proteins ... TCAs [TriCyclic
Antidepressants] act by blocking presynaptic reuptake of both serotonin
and norepinephrine. MAOIs [Mono Amine Oxidase Inhibitors]
act by inhibiting the presynaptic enzyme (monoamine oxidase) ... These
immediate mechanisms of action are not sufficient to explain the delayed
antidepressant effects (typically 2 to 4 weeks). Other unknown mechanisms
must play a role in the successful psychopharmacologic treatment of depression.
... all antidepressants have roughly the same efficacy in treating depression
... [Only] approximately 50% of patients who meet DSM-IV criteria for major
depression will recover with a single adequate trial (at least 6 weeks at a
therapeutic dosage) of an antidepressant." (p. 54 - underline added)
Comment by web-master Douglas Smith: Of course, about half of all
despondent or "depressed" people will feel significantly better in 6 weeks
without "medication," too. What psychiatrists call "other unknown mechanisms"
is just the passage of time.
1999 UPDATES
See quotations in
book review of Your Drug May Be Your Problem by Peter R. Breggin,
M.D., and David Cohen, Ph.D., published in 1999.
No
Prescription for Happiness: Could it be that antidepressants do little more
than placebos?" by Thomas J. Moore, author of Prescription for Disaster,
Boston Globe, October 17, 1999.
2000 UPDATES
There is now evidence SSRI (Selective Serotonin Reuptake
Inhibitor) antidepressants such as Prozac, Paxil, and Zoloft cause brain
damage: In his book Prozac Backlash, published in 2000, Joseph
Glenmullen, M.D., clinical instructor in psychiatry at Harvard Medical School,
says: "In recent years, the danger of long-term side effects has emerged in
association with Prozac-type drugs, making it imperative to minimize one's
exposure to them. Neurological disorders including disfiguring facial and whole
body tics, indicating potential brain damage, are an increasing concern with
patients on the drugs. ... With related drugs targeting serotonin, there is
evidence that they may effect a 'chemical lobotomy' by destroying the nerve
endings that they target in the brain" (p. 8). He compares brain damage that
seems to be caused by SSRI antidepressants (including but not limited to Prozac,
Paxil, and Zoloft) to that caused by neuroleptic/major tranquilizer drugs like
Thorazine, Prolixin, and Haldol. He presents evidence that the so-called
selective serotonin reuptake inhibitors are not selective for serotonin
but affect other chemicals in the brain, including dopamine. For more
information about the book, including excerpts, see the
Barnes & Noble and
Amazon.com websites.
"Most important, the myth of 'accurate
diagnosis' severely narrows treatment options for many psychiatric problems and
has contributed to the excessive use of medication prevalent in our country
today." Edward Drummond, M.D., Associate Medical Director at Seacoast Mental
Health Center in Portsmouth, New Hampshire, in his book The Complete Guide to
Psychiatric Drugs (John Wiley & Sons, Inc., New York, 2000), page 6. Dr.
Drummond graduated from Tufts University School of Medicine and was trained in
psychiatry at Harvard University.
"Nothing has harmed the quality of individual
life in modern society more than the misbegotten belief that human suffering is
driven by biological and genetic causes and can be rectified by taking drugs or
undergoing electroshock therapy. ... If I wanted to ruin someone's life, I
would convince the person that that biological psychiatry is right - that
relationships mean nothing, that choice is impossible, and that the mechanics of
a broken brain reign over our emotions and conduct. If I wanted to impair an
individual's capacity to create empathetic, loving relationships, I would
prescribe psychiatric drugs, all of which blunt our highest psychological
and spiritual functions." Peter R. Breggin, M.D., in the Foreward to Reality
Therapy in Action by William Glasser, M.D. (Harper Collins, 2000), p. xi
(underline added).
"All psychiatric drugs produce severe
biochemical imbalances and related abnormalities by interfering with the normal
brain function." Peter R. Breggin, M.D., in his book
Reclaiming
Our Children (Perseus Books, Cambridge, Mass., 2000), page 140.
"Suppressing Our Children's Signals
Suppose a group of children is standing on the
shore of an island waving their arms crisscross above their heads in the
universal distress signal. Now imagine that a 'hospital ship' spots the
children and comes ashore. Suppose further that the doctor orders the nurses to
give the children Prozac or Ritalin to abort their signals of distress. Now
suppose the ship departs without finding out why the children are alone on the
island, where their parents are, what dangers are surrounding them, or even
whether whey want to be rescued.
"That of course sounds ridiculous. Yet in ways small and large this is
happening throughout the nation. Millions of children are desperately signaling
distress and doctors are sending them home with drugs that suppress their
ability to communicate their distress."
Peter R. Breggin, M.D., in his book
Reclaiming
Our Children (Perseus Books, Cambridge, Mass., 2000), page 142.
2001 UPDATE
U.S. News & World Report, a news magazine, referring to St. John's Wort,
an herbal preparation with supposedly anti-depressant properties, reports that
"Scientists are only beginning to understand how this popular mood-elevator
works in the body." Amanda Spake, U.S. News & World Report,
"Natural Hazards," February 12, 2001, page 43 at 46.
2002 UPDATE
"Neuroleptics have been found to cause a dizzying array of pathological changes
in the brain." Robert Whitaker, Mad in America: Bad Science, Bad Medicine,
and the Enduring Mistreatment of the Mentally Ill, (Perseus - Cambridge,
Massachusetts 2002), p. 191
___________________________
A law firm has much revealing
information about harm caused by Prozac and Zoloft on its web
site:
http://justiceseekers.com. Click on the "Prozac/Zoloft Information" link on
the left edge of the page.
Protocol for Treatment of Benzodiazephine Withdrawal - by Prof. Heather
Ashton, D.M., F.R.C.P. - book by a professor at the University of Newcastle,
School of Neurosciences, Division of Psychiatry, about how to stop taking Xanax,
Valium, Halcion, Atavan, and similar drugs. Available for $20. For information
contact benzo@egroups.com or
YDay548715@aol.com or Geraldine Burns, 3
Searle Road, Boston, Massachusetts 02132.
Article critical of
Prozac.
See also
"Drugging Children
with Ritalin to Curb Hyperactivity" - Antipsychiatry Coalition webmaster
Douglas A. Smith's commentary on a Time magazine cover story titled "The
Age of Ritalin"
 (fluphenazine), Compazine, Stelazine, and Haldol (haloperidol) - and many
others. In terms of their psychological effects, these so-called major
tranquilizers cause misery - not tranquility. They physically, neurologically
blot out most of a person's ability to think and act, even at commonly given
doses. By disabling people, they can stop almost any thinking or behavior the
"therapist" wants to stop. But this is simply disabling people, not therapy.
The drug temporarily disables or permanently destroys good aspects of a person's
personality as much as bad. Whether and to what extent the disability imposed
by the drug can be removed by discontinuing the drug depends on how long the
drug is given and at how great a dose. The so-called major tranquilizer/
antipsychotic/neuroleptic drugs damage the brain more clearly, severely, and
permanently than any others used in psychiatry. Joyce G. Small, M.D., and Iver
F. Small, M.D., both Professors of Psychiatry at Indiana University, criticize
psychiatrists who use "psychoactive medications that are known to have
neurotoxic effects", and speak of "the increasing recognition of long-lasting
and sometimes irreversible impairments in brain function induced by neuroleptic
drugs. In this instance the evidence of brain damage is not subtle, but is
grossly obvious even to the casual observer!" (Behavioral and Brain Sciences,
March 1984, Vol. 7, p. 34). According to Conrad M. Swartz, Ph.D., M.D.,
Professor of Psychiatry at Chicago Medical School, "While neuroleptics relieve
psychotic anxiety, their tranquilization blunts fine details of personality,
including initiative, emotional reactivity, enthusiasm, sexiness, alertness, and
insight. ... This is in addition to side effects, usually involuntary movements
which can be permanent and are hence evidence of brain damage" (Behavioral
and Brain Sciences, March 1984, Vol. 7, pp. 37-38). A report in 1985 in the
Mental and Physical Disability Law Reporter indicates courts in the United
States have finally begun to consider involuntary administration of the
so-called major tranquilizer/antipsychotic/neuroleptic drugs to involve First
Amendment rights "Because...antipsychotic drugs have the capacity to severely
and even permanently affect an individual's ability to think and
communicate" ("Involuntary medication claims go forward", January-February 1985,
p. 26 - emphasis added). In Molecules of the Mind: The Brave New Science of
Molecular Psychology, Professor Jon Franklin observed: "This era coincided
with an increasing awareness that the neuroleptics not only did not cure
schizophrenia - they actually caused damage to the brain. Suddenly, the
psychiatrists who used them, already like their patients on the fringes of
society, were suspected of Nazism and worse" (Dell Pub. Co., 1987, p. 103). In
his book Psychiatric Drugs: Hazards to the Brain, psychiatrist Peter
Breggin, M.D., alleges that by using drugs that cause brain damage, "Psychiatry
has unleashed an epidemic of neurological disease on the world" one which
"reaches 1 million to 2 million persons a year" (op. cit., pp. 109 & 108). In
severe cases, brain damage from neuroleptic drugs is evidenced by abnormal body
movements called tardive dyskinesia. However, tardive dyskinesia is only the
tip of the iceberg of neuroleptic caused brain damage. Higher mental functions
are more vulnerable and are impaired before the elementary functions of the
brain such as motor control. Psychiatry professor Richard Abrams, M.D., has
acknowledged that "Tardive dyskinesia has now been reported to occur after only
brief courses of neuroleptic drug therapy" (in: Benjamin B. Wolman (editor),
The Therapist's Handbook: Treatment Methods of Mental Disorders, Van
Nostrand Reinhold Co., 1976, p. 25). In his book The New Psychiatry,
published in 1985, Columbia University psychiatry professor Jerrold S. Maxmen,
M.D., alleges: "The best way to avoid tardive dyskinesia is to avoid
antipsychotic drugs altogether. Except for treating schizophrenia, they should
never be used for more than two or three consecutive months. What's criminal is
that all too many patients receive antipsychotics who shouldn't" (Mentor, pp.
155-156). In fact, Dr. Maxmen doesn't go far enough. His characterization of
administration of the so-called antipsychotic/anti-schizophrenic/major
tranquilizer/neuroleptic drugs as "criminal" is accurate for all people,
including those called schizophrenic, even when the drugs aren't given long
enough for the resulting brain damage to show up as tardive dyskinesia. The
author of the Preface of a book by four physicians published in 1980, Tardive
Dyskinesia: Research & Treatment, made these remarks: "In the late 1960s I
summarized the literature on tardive dyskinesia ... The majority of
psychiatrists either ignored the existence of the problem or made futile efforts
to prove that these motor abnormalities were clinically insignificant or
unrelated to drug therapy. In the meantime the number of patients affected by
tardive dyskinesia increased and the symptoms became worse in those already
afflicted by this condition. ... there are few investigators or clinicians who
still have doubts about the iatrogenic [physician caused] nature of tardive
dyskinesia. ... It is evident that the more one learns about the toxic effects
of neuroleptics on the central nervous system, the more one sees an urgent need
to modify our current practices of drug use. It is unfortunate that many
practitioners continue to prescribe psychotropics in excessive amounts, and that
a considerable number of mental institutions have not yet developed a policy
regarding the management and prevention of tardive dyskinesia. If this book,
which reflects the opinions of the experts in this field, can make a dent in the
complacency of many psychiatrists, it will be no small accomplishment" (in:
William E. Fann, M.D., et al., Tardive Dyskinesia: Research & Treatment,
SP Medical & Scientific). In Psychiatric Drugs: Hazards to the Brain,
psychiatrist Peter Breggin, M.D., says this: "The major tranquilizers are highly
toxic drugs; they are poisonous to various organs of the body. They are
especially potent neurotoxins, and frequently produce permanent damage to the
brain. ... tardive dyskinesia can develop in low-dose, short-term usage... the
dementia [loss of higher mental functions] associated with the tardive
dyskinesia is not usually reversible. ... Seldom have I felt more saddened or
more dismayed than by psychiatry's neglect of the evidence that it is causing
irreversible lobotomy effects, psychosis, and dementia in millions of patients
as a result of treatment with the major tranquilizers"(op. cit., pp. 70, 107,
135, 146).
(fluphenazine), Compazine, Stelazine, and Haldol (haloperidol) - and many
others. In terms of their psychological effects, these so-called major
tranquilizers cause misery - not tranquility. They physically, neurologically
blot out most of a person's ability to think and act, even at commonly given
doses. By disabling people, they can stop almost any thinking or behavior the
"therapist" wants to stop. But this is simply disabling people, not therapy.
The drug temporarily disables or permanently destroys good aspects of a person's
personality as much as bad. Whether and to what extent the disability imposed
by the drug can be removed by discontinuing the drug depends on how long the
drug is given and at how great a dose. The so-called major tranquilizer/
antipsychotic/neuroleptic drugs damage the brain more clearly, severely, and
permanently than any others used in psychiatry. Joyce G. Small, M.D., and Iver
F. Small, M.D., both Professors of Psychiatry at Indiana University, criticize
psychiatrists who use "psychoactive medications that are known to have
neurotoxic effects", and speak of "the increasing recognition of long-lasting
and sometimes irreversible impairments in brain function induced by neuroleptic
drugs. In this instance the evidence of brain damage is not subtle, but is
grossly obvious even to the casual observer!" (Behavioral and Brain Sciences,
March 1984, Vol. 7, p. 34). According to Conrad M. Swartz, Ph.D., M.D.,
Professor of Psychiatry at Chicago Medical School, "While neuroleptics relieve
psychotic anxiety, their tranquilization blunts fine details of personality,
including initiative, emotional reactivity, enthusiasm, sexiness, alertness, and
insight. ... This is in addition to side effects, usually involuntary movements
which can be permanent and are hence evidence of brain damage" (Behavioral
and Brain Sciences, March 1984, Vol. 7, pp. 37-38). A report in 1985 in the
Mental and Physical Disability Law Reporter indicates courts in the United
States have finally begun to consider involuntary administration of the
so-called major tranquilizer/antipsychotic/neuroleptic drugs to involve First
Amendment rights "Because...antipsychotic drugs have the capacity to severely
and even permanently affect an individual's ability to think and
communicate" ("Involuntary medication claims go forward", January-February 1985,
p. 26 - emphasis added). In Molecules of the Mind: The Brave New Science of
Molecular Psychology, Professor Jon Franklin observed: "This era coincided
with an increasing awareness that the neuroleptics not only did not cure
schizophrenia - they actually caused damage to the brain. Suddenly, the
psychiatrists who used them, already like their patients on the fringes of
society, were suspected of Nazism and worse" (Dell Pub. Co., 1987, p. 103). In
his book Psychiatric Drugs: Hazards to the Brain, psychiatrist Peter
Breggin, M.D., alleges that by using drugs that cause brain damage, "Psychiatry
has unleashed an epidemic of neurological disease on the world" one which
"reaches 1 million to 2 million persons a year" (op. cit., pp. 109 & 108). In
severe cases, brain damage from neuroleptic drugs is evidenced by abnormal body
movements called tardive dyskinesia. However, tardive dyskinesia is only the
tip of the iceberg of neuroleptic caused brain damage. Higher mental functions
are more vulnerable and are impaired before the elementary functions of the
brain such as motor control. Psychiatry professor Richard Abrams, M.D., has
acknowledged that "Tardive dyskinesia has now been reported to occur after only
brief courses of neuroleptic drug therapy" (in: Benjamin B. Wolman (editor),
The Therapist's Handbook: Treatment Methods of Mental Disorders, Van
Nostrand Reinhold Co., 1976, p. 25). In his book The New Psychiatry,
published in 1985, Columbia University psychiatry professor Jerrold S. Maxmen,
M.D., alleges: "The best way to avoid tardive dyskinesia is to avoid
antipsychotic drugs altogether. Except for treating schizophrenia, they should
never be used for more than two or three consecutive months. What's criminal is
that all too many patients receive antipsychotics who shouldn't" (Mentor, pp.
155-156). In fact, Dr. Maxmen doesn't go far enough. His characterization of
administration of the so-called antipsychotic/anti-schizophrenic/major
tranquilizer/neuroleptic drugs as "criminal" is accurate for all people,
including those called schizophrenic, even when the drugs aren't given long
enough for the resulting brain damage to show up as tardive dyskinesia. The
author of the Preface of a book by four physicians published in 1980, Tardive
Dyskinesia: Research & Treatment, made these remarks: "In the late 1960s I
summarized the literature on tardive dyskinesia ... The majority of
psychiatrists either ignored the existence of the problem or made futile efforts
to prove that these motor abnormalities were clinically insignificant or
unrelated to drug therapy. In the meantime the number of patients affected by
tardive dyskinesia increased and the symptoms became worse in those already
afflicted by this condition. ... there are few investigators or clinicians who
still have doubts about the iatrogenic [physician caused] nature of tardive
dyskinesia. ... It is evident that the more one learns about the toxic effects
of neuroleptics on the central nervous system, the more one sees an urgent need
to modify our current practices of drug use. It is unfortunate that many
practitioners continue to prescribe psychotropics in excessive amounts, and that
a considerable number of mental institutions have not yet developed a policy
regarding the management and prevention of tardive dyskinesia. If this book,
which reflects the opinions of the experts in this field, can make a dent in the
complacency of many psychiatrists, it will be no small accomplishment" (in:
William E. Fann, M.D., et al., Tardive Dyskinesia: Research & Treatment,
SP Medical & Scientific). In Psychiatric Drugs: Hazards to the Brain,
psychiatrist Peter Breggin, M.D., says this: "The major tranquilizers are highly
toxic drugs; they are poisonous to various organs of the body. They are
especially potent neurotoxins, and frequently produce permanent damage to the
brain. ... tardive dyskinesia can develop in low-dose, short-term usage... the
dementia [loss of higher mental functions] associated with the tardive
dyskinesia is not usually reversible. ... Seldom have I felt more saddened or
more dismayed than by psychiatry's neglect of the evidence that it is causing
irreversible lobotomy effects, psychosis, and dementia in millions of patients
as a result of treatment with the major tranquilizers"(op. cit., pp. 70, 107,
135, 146).
 institutions as chemical straightjackets - a means of pacifying unruly patients"
(p. 28). I know of two examples of feeble old men in nursing homes who were
barely able to get out of their wheelchairs who were given a
neuroleptic/antipsychotic drug. One complained because he was strapped into a
wheelchair to prevent his attempts to try to walk with his cane. The other was
strapped into his bed at night to prevent him from getting up and falling when
going to the bathroom, necessitating defecating in his bed. Both were so
physically disabled they posed no danger to anyone. But both dared complain
bitterly about how they were mistreated. In both cases the nursing home staffs
responded to these complaints with injections of Haldol - mentally disabling
these men, thereby making it impossible for them to complain. The use of these
damaging drugs on nursing home residents who are not considered to have
psychiatric problems shows that their real purpose is control, not therapy.
Therapeutic claims for neuroleptic drugs are rationalizations without factual
support.
institutions as chemical straightjackets - a means of pacifying unruly patients"
(p. 28). I know of two examples of feeble old men in nursing homes who were
barely able to get out of their wheelchairs who were given a
neuroleptic/antipsychotic drug. One complained because he was strapped into a
wheelchair to prevent his attempts to try to walk with his cane. The other was
strapped into his bed at night to prevent him from getting up and falling when
going to the bathroom, necessitating defecating in his bed. Both were so
physically disabled they posed no danger to anyone. But both dared complain
bitterly about how they were mistreated. In both cases the nursing home staffs
responded to these complaints with injections of Haldol - mentally disabling
these men, thereby making it impossible for them to complain. The use of these
damaging drugs on nursing home residents who are not considered to have
psychiatric problems shows that their real purpose is control, not therapy.
Therapeutic claims for neuroleptic drugs are rationalizations without factual
support. DOWNLOAD
AS PAMPHLET - Click on this link to download a file from which you can print
a copy of this article, "Psychiatric Drugs: Cure or Quackery?," in pamphlet
form. You will need 8Ĺ by 14 inch paper, a printer capable of Hewlett-Packard
Laserjet (PCL 5) emulation, and Corel WordPerfect for Microsoft Windows 95/98.
Printer capable of duplexing (i.e., double-sided printing) is recommended. See
printing instructions.
Most Kinko's Copy shops in the USA and Canada have the needed hardware and
software, often including a duplexing printer, to download and print pamphlets
from this website.
DOWNLOAD
AS PAMPHLET - Click on this link to download a file from which you can print
a copy of this article, "Psychiatric Drugs: Cure or Quackery?," in pamphlet
form. You will need 8Ĺ by 14 inch paper, a printer capable of Hewlett-Packard
Laserjet (PCL 5) emulation, and Corel WordPerfect for Microsoft Windows 95/98.
Printer capable of duplexing (i.e., double-sided printing) is recommended. See
printing instructions.
Most Kinko's Copy shops in the USA and Canada have the needed hardware and
software, often including a duplexing printer, to download and print pamphlets
from this website.